Cervical Radiculopathy
Introduction
Cervical radiculopathy occurs when a nerve in the neck (cervical spine) is pinched or irritated as it branches off of the spinal cord and enters the body. The most common cause is a disc herniation and or other arthritic changes that compress and inflamme the nerve root. Patients often complain of pain that radiates into the shoulder and arm with numbness, tingling and sometimes weakness. Most patients respond to non operative management while those with progressive lesions or neurologic injuries may require surgical treatment.
Causes
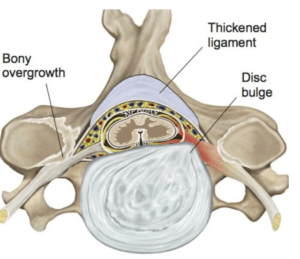
Most cases of cervical radiculopathy are related to disc herniations and or other arthritic changes which accumulate over the years. These include disc protrusions/herniations, thickened ligaments, and enlarged facet joints and bony spurs (figure 1) which compress and irritate the nerve. Instability in the form of spondylolisthesis can further narrow the spinal foramen (the opening the nerve passes through as exits the spine and enters the body). Other less common causes include trauma (fractures), infections, congenital abnormalities, and tumors.
Figure 1
Illustration demonstrating compression and inflammation of the exiting nerve root from a dic herniation in addition to thickened ligamentum flavum and bony spur.
Diagnosis
The diagnosis is made following a detailed history and physical examination by an experienced spine surgeon and confirmed with appropriate imaging studies. Patients with stenosis compressing a nerve root frequently describe arm pain, numbness, tingling and or weakness. Larger lesions can compress the spinal cord producing myelopathy with symptoms including bilateral arm pain, intrinsic hand weakness (dropping objects, difficulty opening jars), numbness (difficulty with fine objects and jewelry), lower extremity weakness or balance problems. Physical exam findings include decreased neck motion with arm pain (+ Spurling), numbness, weakness, and abnormal reflexes. Clinical diagnosis is confirmed with imaging studies especially MRI which best demonstrates spinal anatomy and any correlating neurologic compression. The MRI is non invasive and does not involve radiation (x-ray energy). Some patients are unable to have an MRI due to presence of a pacemaker or other metallic (iron based) loose bodies. In these cases a CT myelogram, which involves injecting a contrast dye into the spinal canal to outline the nerves, will provide good visualization of the spine and stenotic lesions.
Non operative treatment
Most patients will improve with non operative treatment over 4-8 weeks. This includes activity modification to avoid activities that aggravate and inflame the irritated nerve. A soft collar can provide some support with activities that aggravate radicular symptoms. NSAIDs and possible steroid injections including epidural steroids can decrease pain and inflammation and facilitate rehabilitative efforts. Patients with severe pain my require temporary use of narcotics (oxycodone, tramadol, hydrocodone) or muscle relaxants in the presence of muscle spasm. Once the pain and neurologic symptoms improve physical therapy (PT) is very helpful to improve neck motion and strength and increase activities and functional abilities. Therapy also helps educate patients regarding proper body mechanics and posture. PT may also other modalities including ice, heat, ultrasound, TENs unit, and massage. Patients are then instructed in developing a home exercise program that includes core range of motion and strengthening exercises as well as low impact aerobic exercise (swimming, water aerobics, stationary bike, elliptical, etc).
Patients with chronic nerve pain can be treated with “anticonvulsant” medications including gabapentin (Neurontin), pregabalin (Lyrica), topiramate (Topamax) which are thought to act by preventing abnormal increases in brain activity (usually through Na or Ca channels).
Antidepressants such as nortriptyline and duloxetine (Cymbalta) may also be helpful for patients with chronic pain by modulating pain transmission in the central nervous system.
Operative Treatment
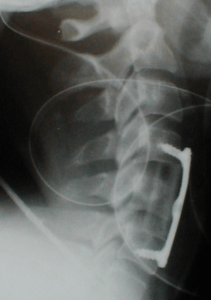
Surgical treatment is the best option for patients with neurologic deficits or those who fail to improve with adequate non operative treatment. Surgical treatment involves removing the compressive lesions (disc herniation and spurs). Disc herniations are treated by an anterior discectomy to decompress the nerves and or spinal cord and fusion and instrumentation to stabilize the spine, ACDFI (figure 3).
Figure 2
Patient with herniated discs at two levels treated two level anterior discectomy, fusion (ACDF)with fibular strut allograft, and instrumentation with plate fixation C4-6.
A small number of patients will have cervical radiculopathy from a soft disc herniation in the posterolateral corner of the spinal canal. These patients may be candidates for minimally invasive spine surgery (MISS) with a foraminotomy and discectomy through a posterior, endoscopic approach. This procedure has the adbatage of relieving the nerve compression and pain while avoiding the extra surgery and loss of motion associated with a fusion procedure. Surgery for cervical radiculopathy is one of the most successful orthopaedic procedures with good to excellent results in the majority (>90%) of patients. Outcome studies demonstrate similar quality of life (QOL) scores compared to total hip and knee arthroplasty and superior cost utility (QALY).
Further Information
- Handout about Herniated Lumbar
- View Case Study 12 about 53 yo male with cervical stenosis and myelopathy treated with anterior decompression and fusion
