Spinal Stenosis
Spinal Stenosis Treatment Palm Beach County
Spinal stenosis is an abnormal narrowing of the spinal canal, which is the passageway for the spinal cord, and nerve roots though the spine (diagram 1). Stenosis can affect any portion of the spine but most commonly involves the lumbar spine (low back), followed by the cervical spine (neck), and less commonly the thoracic spine (mid back). Symptoms may include pain, numbness, paresthesias (or pins and needles sensations), and loss of motor control. This page will explain how spinal stenosis occurs, as well as spinal stenosis treatment options right here in Palm Beach County, including Fort Lauderdale, Delray Beach and Boca Raton, FL.
Figure 1
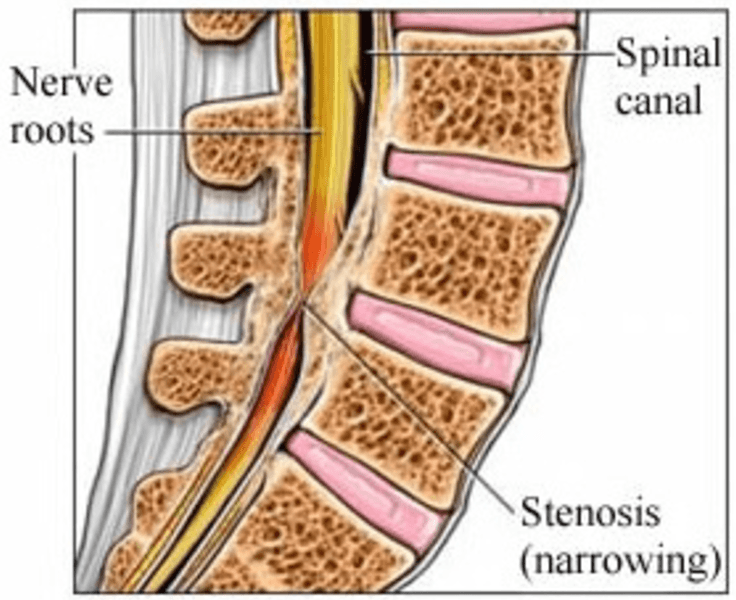
Although lumbar stenosis is more common, cervical and thoracic stenosis are more dangerous as they can lead to spinal cord damage and even paralysis. Stenosis is usually the result of cumulative degenerative changes over the years and becomes more prevalent with age. Stenosis, however, can also be due traumatic injuries, acute disc herniations, and congenital abnormalities.
Lumbar stenosis
Lumbar stenosis is one of the most common conditions of the aging spine affecting up to 8-11% of the population, and an estimated 2.4 million Americans by 2021. Stenosis is usually due to wear and tear changes to the spine, which accumulate over the years. These include disc protrusions and herniations, enlarged, arthritic facet joints, and thickened, hypertrophied ligaments (diagram 2) These changes can narrow the central canal (central canal stenosis) pinching the bundle of nerve roots passing through the spine or they can narrow the small foramen (foraminal stenosis) pinching isolated nerve roots as they exit the spine.
Figure 2
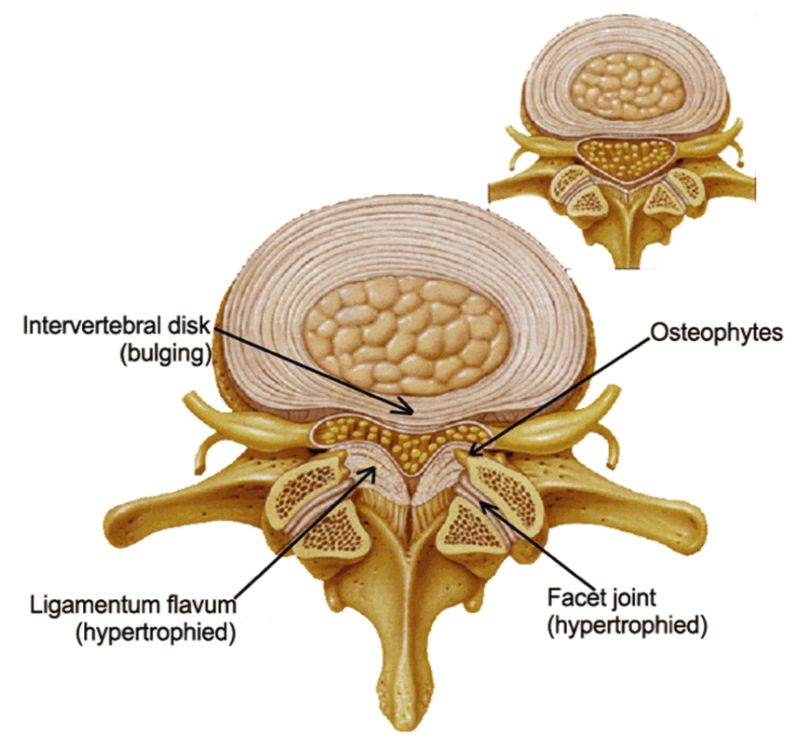
Cross section of the spine illustrating how disc bulging, facet and ligament enlargement (hypertrophy) narrow the spinal canal and compress the associated nerve roots.
The compression of nerve roots can produce a constellation of symptoms described as neurogenic claudication. This typically includes pain and fatigue in the back, which often radiates into the buttocks and legs and is aggravated by standing and walking but relieved by sitting or leaning forward on a cart. This may also include numbness, pins or needles sensation (paresthesias), weakness, and muscle cramping. Although these symptoms may wax and wane over time they tend to worsen over the long term as the degeneration progresses. In addition, these wear and tear changes can produce mechanical back pain from the arthritis itself, which is typically worse in the mornings and aggravated by activities and even weather changes.
Diagnosis
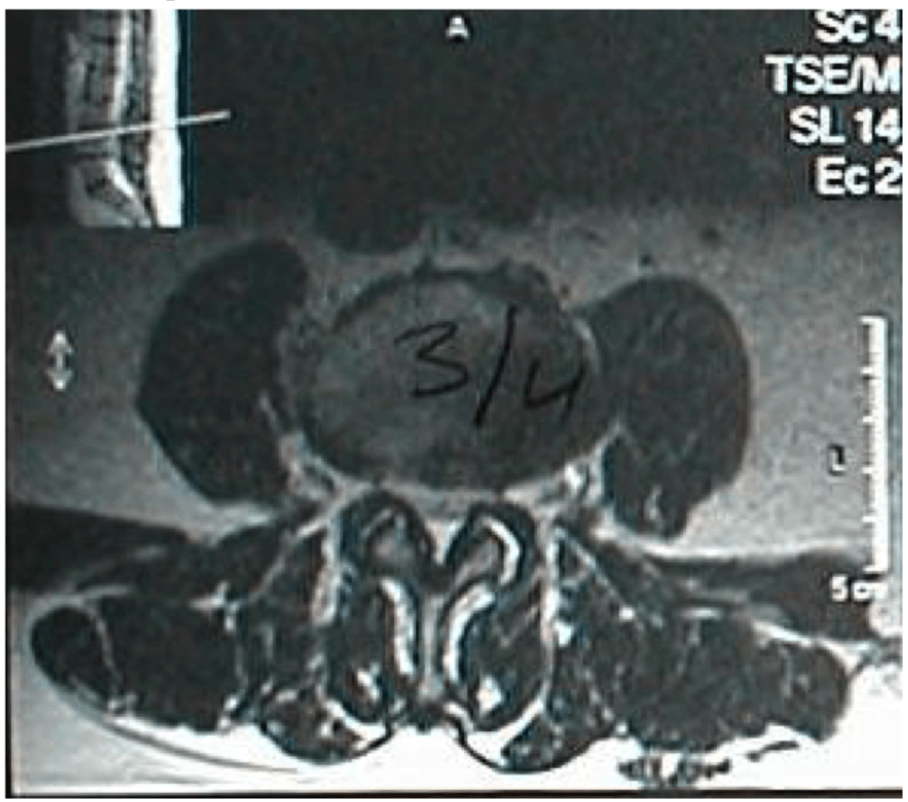
An orthopedic surgeon can make the diagnosis based on a detailed history and physical examination, which is then confirmed with appropriate imaging studies. Magnetic Resonance Imaging (MRI) provides a very detailed visualization of spinal anatomy including any degenerative changes and resulting stenosis. The MRI is non invasive and does not involve radiation (x-ray energy). Some patients are unable to have an MRI due to presence of a pacemaker or other metallic (iron based) loose bodies. In these cases a CT myelogram, which involves injecting a contrast dye into the spinal canal to outline the nerves, will provide good visualization of the spine and stenotic lesions. It’s important for the evaluating orthopedic surgeon to exclude other conditions that produce symptoms similar to stenosis including hip arthritis, vascular stenosis (claudication), and lesions of the cervical and less frequently thoracic spine.
Figure 3
Nonoperative Treatment
The majority of patients with lumbar stenosis are able to manage their condition with nonoperative treatment. This begins with activity modification to avoid activities that aggravate and inflame the “arthritis” and stenosis such as prolonged standing, walking, and extension based activities. Physical therapy (PT) is very helpful to improve trunk motion and strength and increase activities and functional abilities. Therapy also helps educate patients regarding proper body mechanics and posture and correct any forward leaning posture commonly seen in patients with stenosis. PT may also include ice, heat, ultrasound, TENs unit, and other modalities. Patients are then instructed in developing a home exercise program that includes core range of motion and strengthening exercises as well as low impact aerobic exercise (swimming, water aerobics, stationary bike, elliptical, etc). The long-term goal should be an aerobic exercise regimen 3-4 times/week with target heart rate of 75% of maximum. As a general rule, maximum heart rate is estimated as 220 minus age.
Intermittent “flare ups” of fatigue and pain from stenosis is, in part, related to inflammation of the arthritic degenerative changes and stenotic lesions. NSAIDs (ibuprofen, naproxen, Celebrex, etc) can be helpful decreasing the associated inflammation and swelling and thereby relieve pain. In addition, steroid injections at the level of stenosis can be very effective in relieving acute episodes of pain and inflammation from spinal stenosis. These include epidural steroid injections (either through a intra-laminar or trans-foraminal approach) in which the steroid is injected into the epidural space (into the spinal canal but outside the tube of nerves) under fluoroscopic (x-ray) imaging (figure 4).
Figure 4
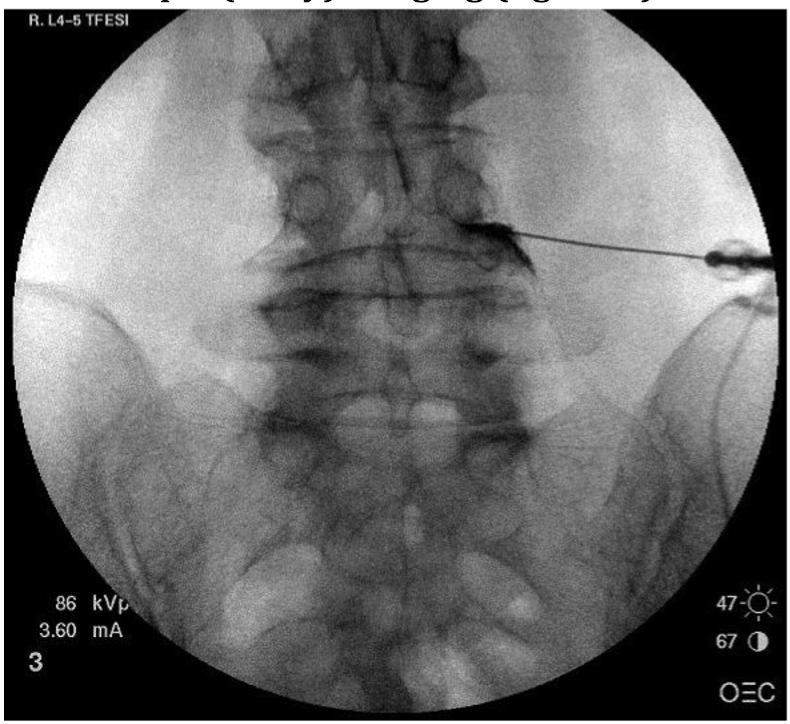
A fluoroscopic (x-ray) image demonstrating placement of the needle into the epidural space and flow of contrast material along the course of the exiting nerve root and into the spinal canal. This was performed at the right side of the L4/5 level and outlines the L4 nerve root.
Patients with more chronic back and leg pain can be treated with “anticonvulsant” medications including gabapentin (Neurontin), pregabalin (Lyrica), topiramate (Topamax) which are thought to act by preventing abnormal increases in brain activity (usually through Na or Ca channels).
Antidepressants such as nortriptyline and duloxetine (Cymbalta) may also be helpful for patients with chronic pain by modulating pain transmission in the central nervous system. Finally, severe bouts of pain can be treated in the short term with narcotic medications (Tramadol, hydrocodone, oxycodone) but should be avoided in the long term due to the accumulative risks of side effects. A carefully tailored, multi modal approach will successfully control symptoms over the long term (2-10 years) for the majority of patients with spinal stenosis (60-80%) and the majority of these (50-70%) will have significant improvement of their pain.
Spinal Stenosis Treatment in Boca Raton – Operative
For those patients with persistent symptoms despite adequate nonoperative treatment surgery can successfully decompress the spine, relieve pain, and improve functional abilities in the great majority of cases. Surgical treatment involves removal of the stenotic lesion; this usually includes removing a portion of lamina (the roof of the spinal canal), facet joints (the upper corner of the canal), and disc herniations or bone spurs (usually along the floor and bottom corners of the canal) at each stenotic level.
This can be done through a minimally invasive spine surgery (MISS ) approach in more localized lesions with less severe stenosis and open approaches for more involved cases. The presence of instability, due to removal of more than 50% of the facet joints or underlying spondylolisthesis usually requires stabilization with a fusion procedure (XLIF, TLIF, PLFI). Surgery for spinal stenosis is one of the most successful orthopaedic procedures with good to excellent results in the majority (>90%) of patients. Outcome studies demonstrate similar quality of life (QOL) scores following spinal decompression compared to total hip and knee arthroplasty and superior cost utility (QALY).
Spinal Stenosis Treatment in Fort Lauderdale and Boca Raton – Further information
If you have back pain or believe you have spinal stenosis, please make an appointment with our Orthopedic Spine Surgeon in Fort Lauderdale or Delray Beach. Alternatively, feel free to read about the two case studies below, which both involved forms of spinal stenosis:
Case 11: 61 yo male with severe cervical stenosis and myelopathy
References
1. Lurie JD, Tosteson TD, Abdu WA, et al. Long-term outcomes of lumbar spinal stenosis. Spine 2015; 40(2): 63-76.
2. Amundsen T, Weber H, Nordal HJ, et al. Lumbar spinal stenosis: conservative or surgical management? : A prospective 10-year study. Spine. 2000; 25(11):1424- 1435; discussion 1435-1426.
