Spondylolysis
Spondylolysis is a common pathologic lesion present in 5-7% of individuals in the US population – (Figure 4a).
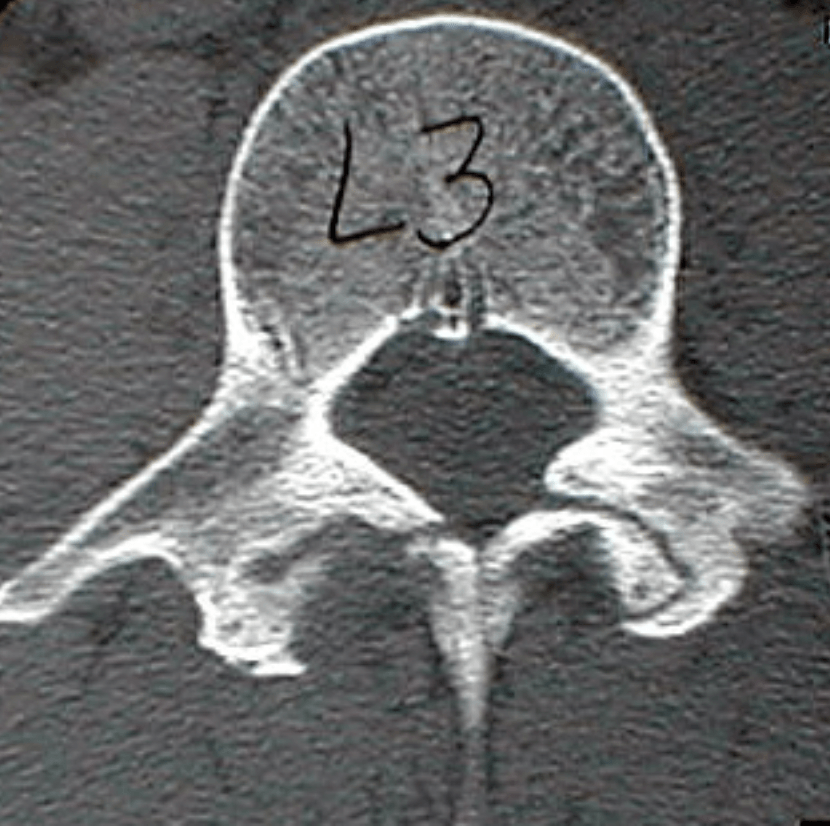
Figure 4a Note the chronic lytic lesions bilaterally characterized by their sclerotic margins. The defect itself is filled with fibrocartilaginous tissue which prevents healing and must be removed.
While many of these may be asymptomatic others may interfere with sporting activities, work, or activities of daily living. Many individuals with acutely painful spondylolytic lesions will improve with nonoperative management including activity restriction, NSAIDS, and bracing and frequently return to full activity. Others may require surgical treatment for continued pain and occasional neurologic symptoms. Many more may improve with cessation of high school sports/vigorous activities only to return decades later with worsening low back pain and accompanying disc degeneration and or progression to spondylolisthesis. Various techniques have been described to surgically treat spondylolysis including bone graft repair with internal fixation (wires, screws, and hook screw constructs) ––. Each of these methods has been affected by technical difficulties and high complication rates including construct loosening and nonunion. Others treat spondylolysis with posterior fusion which sacrifices the motion segment and leads to higher levels of stress and degeneration at the adjacent levels. We recently reported our results treating the pars defect with rigid fixation using a pedicle screw-hook (claw) construct (Figure 5a).
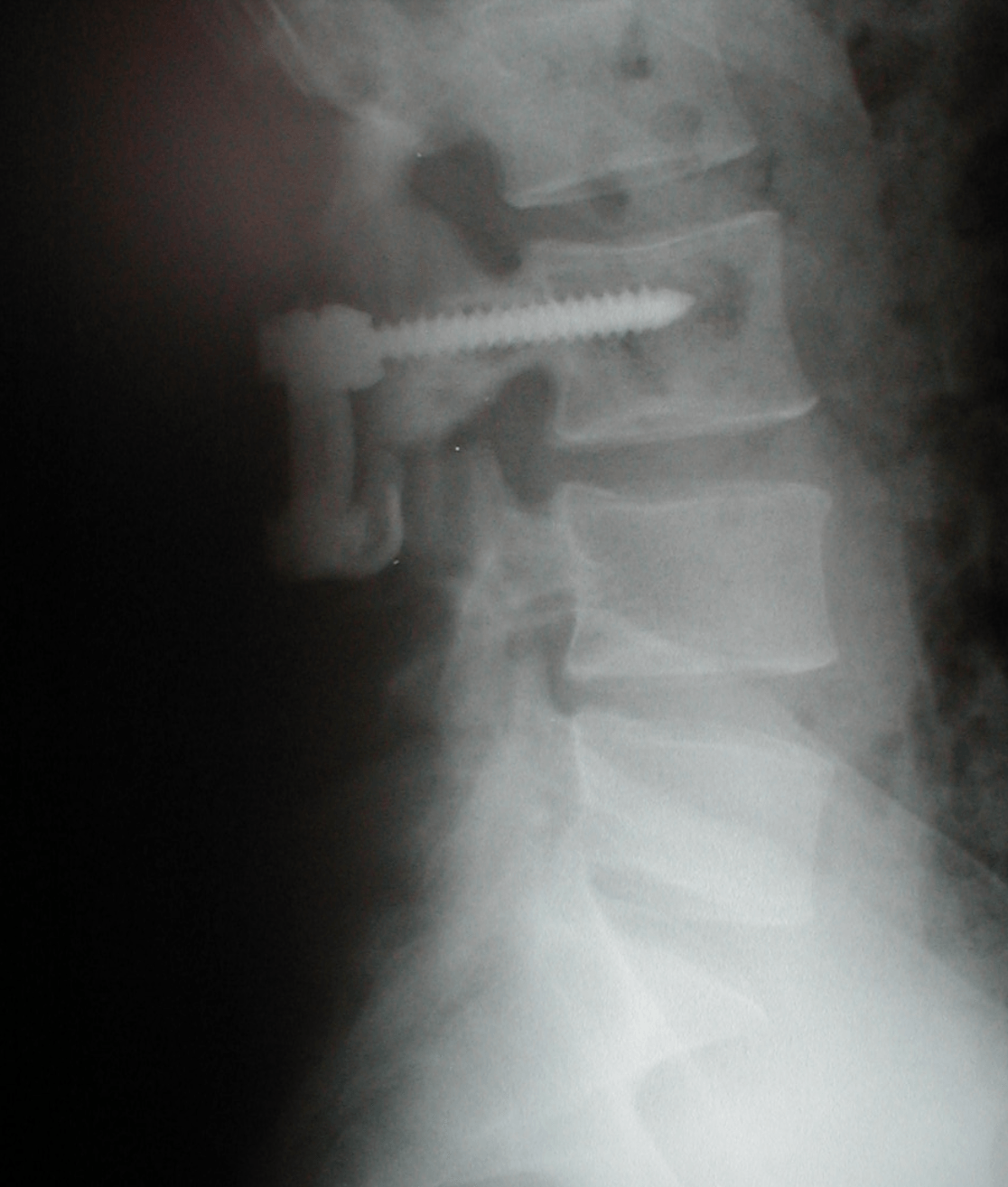
Figure 5a Lateral xray demonstrating the pedicle screw-laminar hook (claw) construct.
We prospectively evaluated the clinical and radiological results of pars repair of 10 lesions in 8 consecutive patients who failed nonoperative treatment including bracing. Surgical technique included debridement of the pseudoarthosis, bone grafting (iliac crest autograft), and rigid stabilization with a pedicle screw-sublaminar hook (claw) construct. (Figures 6a and 7a).
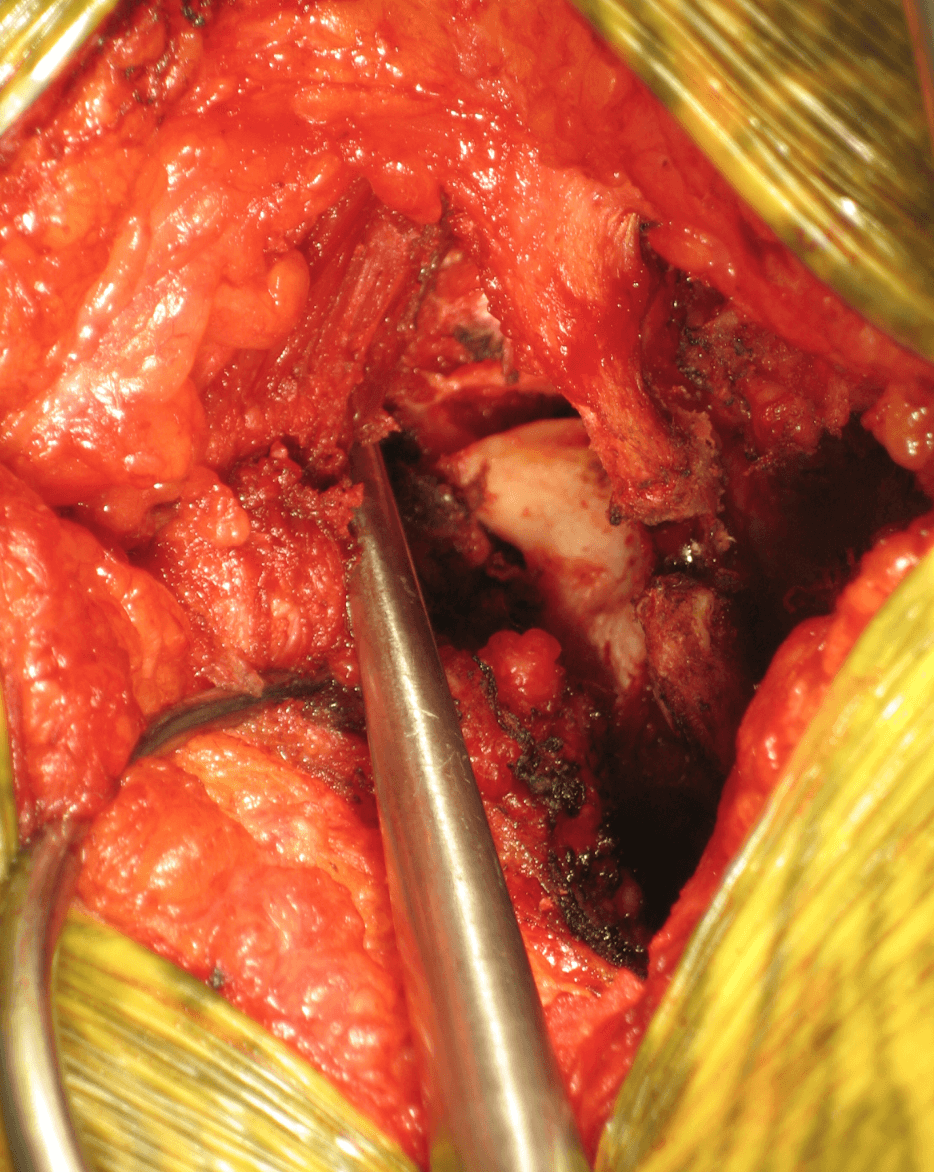
Figure 6a The stress fracture on the left has been debrided of fibrocartilaginous debris and the remaining defect is seen. The right stress fracture has not yet been debrided and is characterized by an inflammatory pannus of tissue overlying the fracture itself. This inflammatory tissue must be removed before the margins of the fracture can be visualized and debrided.
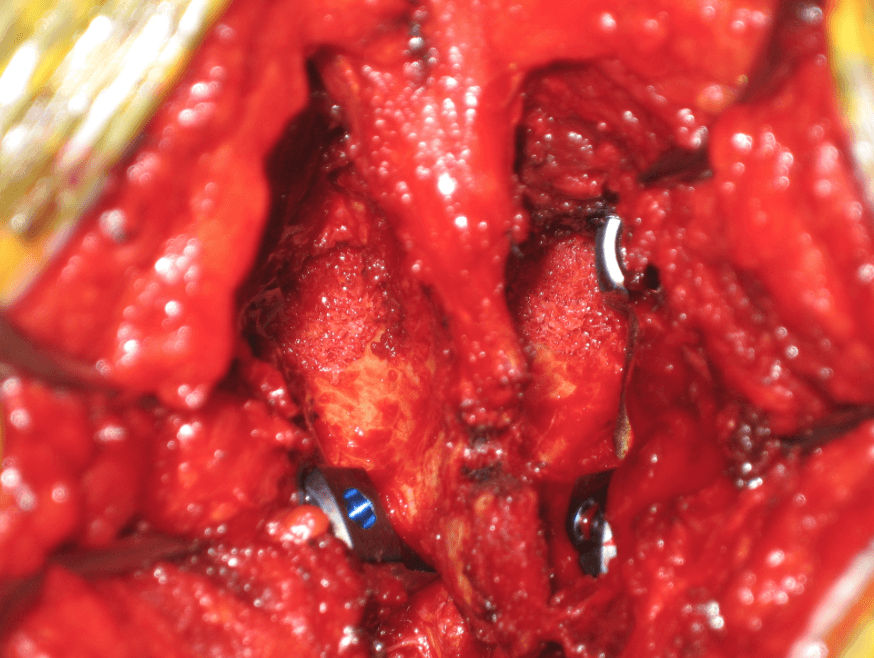
Figure 7a The stress fractures have been debrided and then packed with autologous bone graft. The surrounding posterior elements (lamina, pars, base of pedicle and transverse process) have been decorticated.
Concomitant diagnosis included an adjacent spondylolysis (2), spondylolisthesis (3), and DDD/HNP (4). Postoperative treatment included TLSO bracing for 3 months, physical therapy (aerobic conditioning and core strengthening) at 3 months, and sport specific rehabilitation thereafter. Outcome measures demonstrated an improvement from preop to 1 yr postop in Oswestry 2.0 (5.2-1), Roland Morris (7.4-0) VAS (8.3-0) and SF-36. Xrays with flexion/extension and CT scan demonstrate solid pars repair in 10/10 lesions (Figure 8a).

Figure 8a Axial CT scan through the level of the pars 6 months postoperatively demonstrating complete bony healing of the lytic defect. At this point the patient, a Division I college tight end, returned to complete the full season without limitation or back pain.
All patients returned to a full level of activity including contact sports within 6 months (two football players had BMP to increase rate of healing and permit competition within 6 months). We strongly recommend primary repair of spondylolysis in patients who have continued symptoms despite nonoperative treatment as it has excellent clinical results and fusion rates, restores physiologic motion and biomechanics, and permits early return to full activity level (including contact sports).
